When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
Snoring and Sleep
A closer look at what snoring is as well as its causes, consequences, and treatments
- The vibration of relaxed throat tissues during sleep causes snoring.
- Pregnancy, weight gain, sedative medications, and congestion can contribute to snoring.
- Snoring related to sleep apnea is often accompanied by other symptoms, like gasping for air and daytime fatigue.
- Talk to your doctor about snoring solutions, including lifestyle changes, mouthpieces, and PAP therapy.
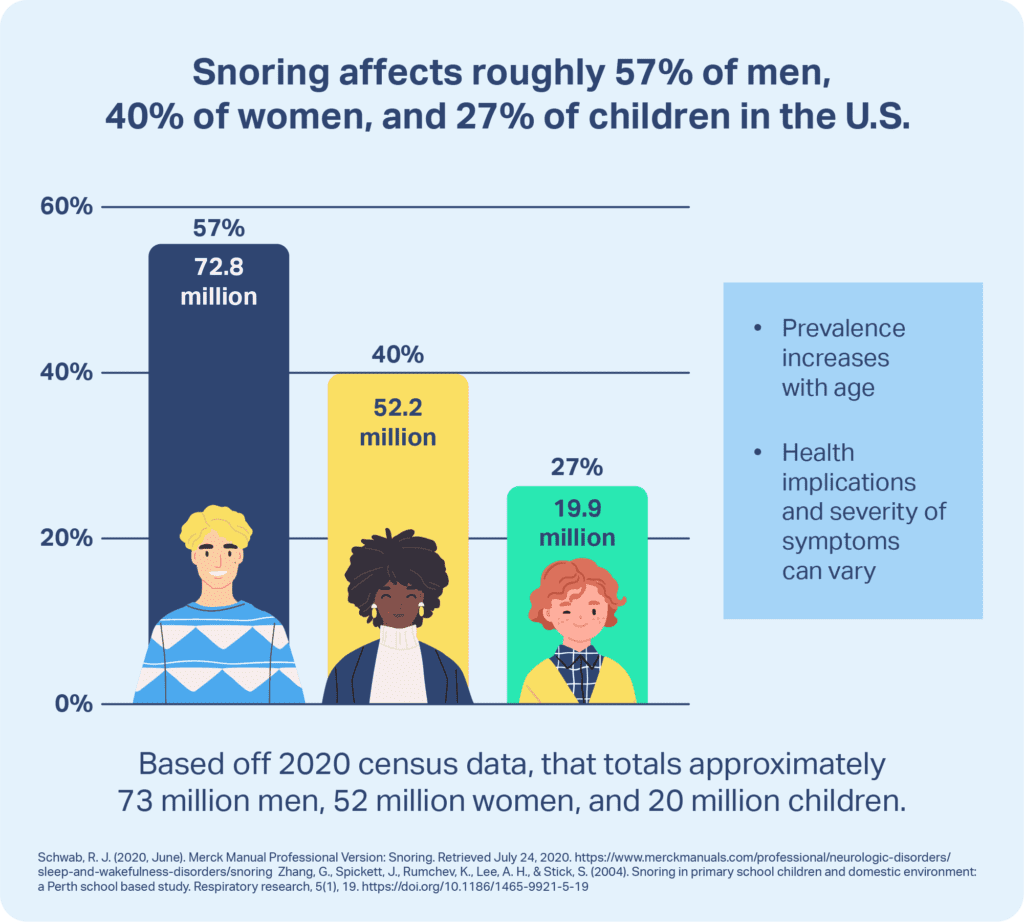
Snoring is a widespread issue, but its severity and health implications can vary. Snoring can be light, occasional, and unconcerning, or it may be the sign of a serious underlying sleep-related breathing disorder. More than a quarter of adults experience snoring on a regular basis.
Knowing the basics about snoring, including what causes it, when it is dangerous, and how to treat it, can facilitate better health and eliminate a common cause of sleep complaints.
What Causes Snoring?
Snoring is caused by the rattling and vibration of tissues near the airway in the back of the throat. During sleep, the muscles loosen, narrowing the airway. As a person inhales and exhales, the moving air causes the tissue to flutter and make noise.
Some people are more prone to snoring because of the size and shape of the muscles and tissues in their neck. In other cases, excess relaxing of the tissue or narrowing of the airway can lead to snoring. Examples of risk factors that contribute to a higher risk of snoring include:
- Obesity
- Alcohol consumption
- Use of sedative medications
- Chronic nasal congestion
- Large tonsils, tongue, or soft palate
- Deviated septum or nasal polyps
- Jaw that is small or set back
- Pregnancy
What’s the Difference Between Snoring and Sleep Apnea?
Obstructive sleep apnea (OSA) is a breathing disorder in which the airway gets blocked or collapses during sleep, causing repeated lapses in breath.
Snoring is one of the most common symptoms of OSA , but not all people who snore have OSA. OSA-related snoring tends to be loud and sound as if a person is choking, snorting, or gasping .
OSA disturbs sleep and often disrupts the balance of oxygen and carbon dioxide in the body. More mild snoring, often called primary snoring, occurs frequently but does not provoke these other effects.
Is Snoring Dangerous?
Whether snoring is dangerous depends on its type, severity, and frequency.
- Light snoring: Light, infrequent snoring is normal and does not typically require medical testing or treatment. Its main impact is on a bed partner or roommate who may be bothered by the occasional noise.
- Primary snoring: Primary snoring occurs more than three nights per week. Because of its frequency, it is more disruptive to bed partners. However, it is not usually seen as a health concern unless there are signs of sleep disruptions or sleep apnea, in which case diagnostic tests may be necessary.
- Snoring related to obstructive sleep apnea: OSA-associated snoring is more worrisome from a health perspective. If OSA goes untreated, it can have major implications for a person’s sleep and overall health. Unchecked OSA is associated with dangerous daytime drowsiness, and serious health conditions including cardiovascular issues, high blood pressure, diabetes, stroke, and depression.
When Should You See a Doctor About Snoring?
Many instances of snoring are benign, but it is important to talk with a doctor if there are signs of potential sleep apnea:
- Snoring that occurs three or more times per week
- Very loud or bothersome snoring
- Snoring with gasping, choking, or snorting sounds
- Obesity or recent weight gain
- Daytime drowsiness
- Lack of focus or mental sharpness
- Morning headaches and congestion
- High blood pressure
- Nighttime teeth grinding
- Frequent nighttime urination
If you have noticed any of these signs, it is important to address the issue with a doctor who can determine if additional testing or treatment is necessary.
How Do I Know if I’m Snoring When I Sleep Alone?
Unless someone else tells them, most people who snore are not aware of it. This may be part of why sleep apnea is underdiagnosed .
If you sleep alone, it may be helpful to set up a recording device. It could be a simple tape recorder or one of many smartphone apps, but the apps have the advantage of analyzing sound patterns for you to detect likely episodes of snoring. It is best to record for multiple nights since snoring may not occur every night. That being said, apps do not aid in the diagnosis of OSA.
It is also important to look for other signs related to disrupted sleep such as noticeable daytime sleepiness, fatigue, problems with attention or thinking, or unexplained mood changes.
Take Our Quiz to Know Your Sleep Apnea Risk
To understand if you could have sleep apnea, take our short quiz below to see if you exhibit any signs.
What Treatments Can Help Stop Snoring?
Treatment depends on the nature of the snoring and the types of problems it causes.
For people with infrequent or primary snoring, treatment may not be necessary unless it is disturbing the person’s sleep or the sleep of someone they live with. In those cases, treatments tend to be simpler and less invasive. People with sleep apnea usually need more involved treatment.
Types of treatments include lifestyle changes, anti-snoring mouthpieces, mouth exercises, positive airway pressure (PAP) devices, and surgery. A person’s physician is in the best position to describe pros and cons of any treatment in their specific case.
Lifestyle Changes
Lifestyle changes can help stop snoring, and in some cases, other treatments may not be necessary. Even when other treatments are prescribed, lifestyle changes are often still recommended.
- Maintaining a healthy weight: Being overweight or obese are risk factors for snoring and sleep apnea, so keeping a healthy weight can be an important step against snoring.
- Limiting use of alcohol and sedatives: Alcohol is a frequent promoter of snoring, and sedative medications can trigger snoring as well.
- Adjusting your sleep position: Sleeping on your back makes it easier for your airway to become obstructed. It may take time to get used to a different sleep position, but it can be a helpful change.
- Raising the head of your bed: Elevating the top part of your bed with risers, a wedge pillow, or an adjustable frame may help reduce snoring.
- Reducing nasal congestion: Taking steps to eliminate allergies or other sources of nasal congestion can combat snoring. Breathing strips that go over the nose may help open your nasal passages during the night, as well as internal nasal expanders.
Anti-Snoring Mouthpieces
An anti-snoring mouthpiece helps hold your tongue or jaw in a stable position to prevent airway blockages while you sleep. There are two main types of anti-snoring mouthpieces.
- Mandibular advancement devices: These work by holding the lower jaw forward. Many are adjustable so that you can find a more comfortable and effective fit.
- Tongue retaining devices: These mouthpieces help hold the tongue in place so that it does not slide back toward your throat.
CPAP is still considered the gold standard treatment for sleep apnea. However, while some people can use a CPAP machine comfortably, others find the device bothersome, especially if the machine is loud or if the mask fits poorly. Custom-fitted oral appliances are often a suitable alternative for OSA patients who cannot tolerate CPAP . Mandibular advancement devices, specifically, have been shown to be effective in treating snoring and mild to moderate OSA. It is important to consult a doctor to develop the best treatment plan.
Mouth Exercises
Slackening of the muscles around the airway makes it more likely for a person to snore. Exercises to strengthen the mouth, tongue, and throat can counteract this, building muscle tone to reduce snoring.
Anti-snoring mouth exercises have shown most effectiveness in people with mild snoring and usually must be completed daily over a period of two or three months.
Positive Airway Pressure Devices
Continuous positive airway pressure (CPAP) machines are one of the most common treatments for sleep apnea in adults. They pump pressurized air through a hose and a mask and into the airway, preventing it from being obstructed. Bilevel positive airway pressure (BiPAP or BPAP) machines are similar but have different pressure levels for inhaling and exhaling. Auto-adjusting positive airway pressure (APAP) machines respond to breathing patterns and vary the pressure as needed.
CPAP, BiPAP, and APAP machines are often effective in treating sleep apnea and associated snoring. You need a prescription to get these devices, and they must be calibrated to suit your breathing. For that reason, it is important to work with a sleep technician to get started with a PAP device.
Wearing a PAP mask may be uncomfortable at first, but most people get used to it and find that using the device noticeably reduces snoring and improves sleep.
Surgery
In adults, surgery is rarely the first-line treatment for snoring or sleep apnea, but it may be an option if other approaches are not effective.
One type of surgery, called uvulopalatopharyngoplasty, widens the airway by adjusting or removing nearby tissue. Surgery can also address nasal polyps, a deviated septum, or other blockages of the nasal passages.
Other types of less-invasive surgeries have been developed, but to date there is limited evidence from clinical trials regarding their benefits and downsides.
References
6 Sources
-
Schwab, R. J. (2022, May). Snoring. Merck Manual Consumer Version., Retrieved February 8, 2023, from
https://www.merckmanuals.com/home/brain,-spinal-cord,-and-nerve-disorders/sleep-disorders/snoring -
A.D.A.M. Medical Encyclopedia. (2021, July 19). Snoring – adults. MedlinePlus., Retrieved February 8, 2023, from
https://medlineplus.gov/ency/patientinstructions/000720.htm -
Strohl, K. P. (2022, October). Sleep apnea. Merck Manual Consumer Version., Retrieved February 8, 2023, from
https://www.merckmanuals.com/home/lung-and-airway-disorders/sleep-apnea/sleep-apnea -
Kline, L. R. (2023, January 13). Clinical presentation and diagnosis of obstructive sleep apnea in adults. In N. Collop (Ed.). UpToDate., Retrieved February 8, 2023, from
https://www.uptodate.com/contents/clinical-presentation-and-diagnosis-of-obstructive-sleep-apnea-in-adults -
Auckley, D. (2022, November 18). Obstructive sleep apnea and other sleep disorders in hospitalized adults. In R. Benca & N. Collop (Eds.). UpToDate., Retrieved February 8, 2023, from
https://www.uptodate.com/contents/sleep-disorders-in-hospitalized-adults-evaluation-and-management -
Ramar, K., Dort, L. C., Katz, S. G., Lettieri, C. J., Harrod, C. G., Thomas, S. M., & Chervin, R. D. (2015). Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: An update for 2015. Journal of Clinical Sleep Medicine, 11(7), 773–827.
https://pubmed.ncbi.nlm.nih.gov/26094920/